Understanding our blood’s composition is akin to deciphering the body’s hidden language in the latest healthcare industry. Imagine a scenario where the secret messages within blood cells could unlock crucial insights into our health. This guide explores the world of automatic hematology analyzers, illuminating their pivotal role in decoding blood counts and unraveling the mysteries within.
Table of Contents
The Vital Role of Blood Analysis
Picture this: A patient awaiting crucial diagnostic information, a clinician seeking rapid insights for effective treatment, or a researcher delving into the depths of hematological mysteries. In each scenario, the analysis of blood holds the key. Automatic hematology analyzers emerge as unsung heroes, offering efficiency and precision in unraveling the complexities of blood composition.
Demystifying Blood Counts
Automatic hematology analyzers play a pivotal role in providing comprehensive information about the cellular components of blood through a process known as a complete blood count (CBC). Understanding the key components and parameters reported by these analyzers is essential for healthcare professionals and individuals seeking insights into their blood health. Let’s demystify the blood counts obtained from automatic hematology analyzers:
1. Red Blood Cell (RBC) Count
Definition: The number of red blood cells per microliter of blood.
Significance: Reflects the oxygen-carrying capacity of the blood and helps diagnose conditions such as anemia.
2. White Blood Cell (WBC) Count
Definition: The total number of white blood cells per microliter of blood.
Significance: Indicates the body’s immune response and aids in the diagnosis of infections, inflammatory disorders, and leukemia.
3. Hemoglobin (Hb) Concentration
Definition: The amount of hemoglobin in a given volume of blood.
Significance: Measures the blood’s oxygen-carrying capacity and is crucial for assessing anemia and other hemoglobin-related disorders.
4. Hematocrit (Hct) Level
Definition: The percentage of blood volume occupied by red blood cells.
Significance: Complements the RBC count in evaluating anemia and monitoring conditions affecting blood volume.
5. Platelet Count
Definition: The number of platelets per microliter of blood.
Significance: Essential for assessing blood clotting ability and diagnosing disorders such as thrombocytopenia or thrombocytosis.
6. Mean Corpuscular Volume (MCV)
Definition: The average volume of a red blood cell.
Significance: Helps classify anemias based on red blood cell size and aids in identifying nutritional deficiencies.
7. Mean Corpuscular Hemoglobin (MCH)
Definition: The average amount of hemoglobin in a red blood cell.
Significance: Provides insights into the amount of hemoglobin carried by individual red blood cells.
8. Mean Corpuscular Hemoglobin Concentration (MCHC)
Definition: The concentration of hemoglobin in a red blood cell.
Significance: Evaluates the average hemoglobin concentration and aids in diagnosing hemoglobinopathies.
9. Red Cell Distribution Width (RDW)
Definition: Measures the variation in red blood cell size.
Significance: Indicates the degree of anisocytosis (variability in RBC size) and aids in diagnosing different types of anemias.
10. Differential White Blood Cell (WBC) Count
Definition: Breakdown of the types and percentages of white blood cells.
Significance: Helps identify specific immune responses and diagnose various infections or blood disorders.
Interpreting these blood counts requires considering the interplay of multiple parameters and their relation to each other. Automatic hematology analyzers, with their advanced technology, provide quick and accurate results, enabling healthcare professionals to make informed diagnostic and treatment decisions. It’s essential to consult with a healthcare provider for a thorough analysis and interpretation of blood count results in the context of an individual’s overall health.
Check our: Automatic Hematology Analyzer
The Power of Automation: Enter Automatic Hematology Analyzers
From Manual to Automatic: A Technological Leap
Traditionally, blood cell analysis was a manual process, laden with limitations and subject to human error. Automatic hematology analyzers, a beacon of technological advancement, now streamline this process. These sophisticated instruments automate the counting and characterization of blood cells, ensuring not only efficiency but also accuracy in diagnosis.
Working Principle
At a high level, these analyzers use a combination of optical and electrical methods to categorize and count blood cells swiftly. The automation not only reduces the risk of errors but also accelerates the diagnostic process.
The Power of Automation: Enter Automatic Hematology Analyzers
Key Features of Automatic Hematology Analyzers
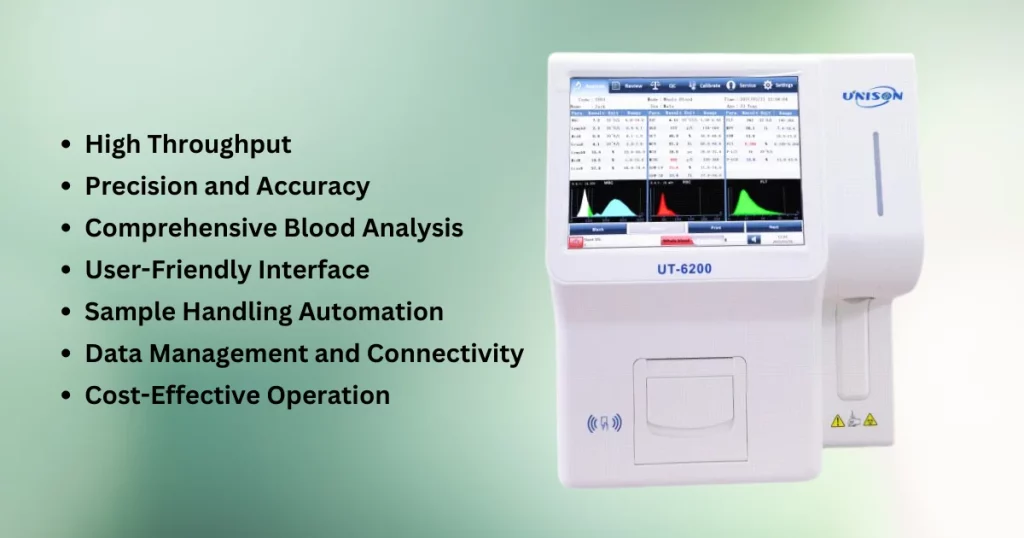
1. High Throughput
- Efficiency: Automatic hematology analyzers can process a large number of blood samples in a relatively short time, enhancing the overall efficiency of laboratory workflows.
- Time Savings: Rapid analysis allows for quicker turnaround times, enabling healthcare professionals to promptly assess and address patient needs.
2. Precision and Accuracy
- Advanced Technology: Leveraging cutting-edge technology, these analyzers offer precise and accurate measurements of various blood parameters, ensuring reliable and consistent results.
- Reduced Variability: Automation minimizes the risk of human error, contributing to the reproducibility and reliability of laboratory data.
3. Comprehensive Blood Analysis
- Complete Blood Count (CBC): Automatic hematology analyzers provide a comprehensive CBC, encompassing key parameters such as red blood cell count, white blood cell count, hemoglobin concentration, and platelet count.
- Differential Analysis: The ability to perform differential white blood cell counts aids in identifying specific cell types, enhancing diagnostic capabilities.
4. User-Friendly Interface
- Intuitive Operation: Designed with user convenience in mind, these analyzers often feature user-friendly interfaces, making them accessible to laboratory technicians with varying levels of expertise.
- Automated Calibration: Some models incorporate automated calibration processes, simplifying instrument maintenance and ensuring optimal performance.
5. Sample Handling Automation
- Automated Sample Preparation: From sample aspiration to analysis, many analyzers automate the entire process, reducing manual intervention and enhancing laboratory efficiency.
- Sample Identification: Integrated barcode scanning and sample tracking systems help prevent errors in sample identification.
6. Data Management and Connectivity
- Digital Records: Automatic hematology analyzers generate digital records of test results, facilitating efficient data management and storage.
- Integration with Laboratory Information Systems (LIS): Seamless connectivity with LIS enables the automatic transfer of results, improving overall laboratory workflow.
7. Cost-Effective Operation
- Resource Optimization: Automation minimizes the need for extensive manual labor, allowing laboratories to optimize their resources and allocate personnel to more complex tasks.
- Reduced Turnaround Time: Faster analysis contributes to increased lab throughput, potentially reducing overall operational costs.
The integration of automatic hematology analyzers into clinical laboratories represents a paradigm shift in diagnostic capabilities. Their ability to deliver rapid, accurate, and comprehensive blood analyses not only expedites medical assessments but also plays a pivotal role in enhancing patient care. As technology continues to advance, these automated systems are poised to further elevate the standards of diagnostic medicine, contributing to improved healthcare outcomes.
Exploring Features and Applications
Automatic hematology analyzers are advanced diagnostic tools designed to streamline and enhance the process of blood analysis. These instruments come with a range of features that contribute to their efficiency and versatility, making them invaluable in various medical settings. Let’s delve into the key features and applications of automatic hematology analyzers:
1. Complete Blood Count (CBC)
Feature: Automatic hematology analyzers provide a comprehensive CBC, including counts of red blood cells (RBCs), white blood cells (WBCs), and platelets.
Application: CBC analysis is fundamental in diagnosing a wide range of conditions, including anemia, infections, and blood disorders.
2. Differential WBC Count
Feature: The ability to differentiate and count various types of white blood cells (neutrophils, lymphocytes, monocytes, eosinophils, and basophils).
Application: A detailed WBC differential aids in identifying specific types of infections, inflammatory conditions, and immune system disorders.
3. Hemoglobin Measurement
Feature: Accurate measurement of hemoglobin levels in blood samples.
Application: Hemoglobin analysis is crucial for diagnosing and monitoring conditions such as anemia and assessing overall oxygen-carrying capacity.
4. Platelet Count and Morphology
Feature: Automatic analyzers assess platelet counts and can also provide information on platelet morphology.
Application: Platelet analysis helps in detecting and monitoring disorders such as thrombocytopenia or thrombocytosis.
5. Reticulocyte Analysis
Feature: Some analyzers offer reticulocyte counts to assess the rate of new red blood cell production.
Application: Reticulocyte counts are valuable in diagnosing and monitoring anemia, as well as evaluating bone marrow function.
6. Comprehensive Data Management
Feature: Advanced data management systems for storing, retrieving, and analyzing patient results.
Application: Efficient data management enhances workflow, facilitates trend analysis, and supports accurate patient diagnosis.
7. Quality Control Functions
Feature: Built-in quality control mechanisms to ensure the accuracy and reliability of results.
Application: Quality control features are essential for meeting regulatory standards and ensuring the precision of diagnostic outcomes.
8. User-Friendly Interface
Feature: Intuitive interfaces with touchscreens and user-friendly menus.
Application: User-friendly interfaces simplify operation, reduce training time, and enhance overall user experience.
9. Automation and Throughput
Feature: High levels of automation for sample processing, reducing manual intervention.
Application: Increased throughput and efficiency, especially in laboratories with high testing volumes.
10. Connectivity and Integration
Feature: Integration with laboratory information systems (LIS) and other devices for seamless data exchange.
Application: Enhanced connectivity supports streamlined laboratory workflows and efficient data sharing.
Automatic hematology analyzers, with their array of features and applications, play a pivotal role in modern healthcare by providing rapid, accurate, and comprehensive blood analysis. These instruments contribute significantly to the diagnosis and monitoring of various medical conditions, ultimately improving patient care and outcomes.
Benefits of Using Automatic Hematology Analyzers

Automatic hematology analyzers offer a myriad of advantages that contribute to their widespread adoption in clinical laboratories and healthcare settings. Here are key benefits associated with the use of these advanced diagnostic instruments:
1. Efficiency and Speed
Benefit: Automatic hematology analyzers streamline the blood analysis process, providing rapid and high-throughput results.
Impact: Increased efficiency enables laboratories to handle a larger volume of samples in a shorter time, leading to quicker diagnosis and treatment decisions.
2. Comprehensive Blood Analysis
Benefit: These analyzers provide a complete blood count (CBC) with differential white blood cell (WBC) counts, hemoglobin levels, platelet counts, and more.
Impact: A comprehensive analysis offers a detailed overview of a patient’s hematological status, aiding in the diagnosis and monitoring of various conditions.
3. Accuracy and Precision
Benefit: Automatic analyzers are equipped with quality control mechanisms to ensure the accuracy and precision of test results.
Impact: Reliable and consistent results contribute to the confidence of healthcare professionals in using the data for patient diagnosis and management.
4. Reduced Manual Intervention
Benefit: Automation minimizes the need for manual sample preparation and handling.
Impact: Reduced manual intervention not only improves workflow efficiency but also lowers the risk of errors associated with manual processes.
5. Advanced Data Management
Benefit: Hematology analyzers come with sophisticated data management systems for storing, retrieving, and analyzing patient results.
Impact: Efficient data management supports better organization of information, facilitates trend analysis, and ensures compliance with regulatory standards.
6. User-Friendly Interfaces
Benefit: Intuitive interfaces, often featuring touchscreens and user-friendly menus, make operation straightforward.
Impact: User-friendly interfaces contribute to ease of use, requiring less training for laboratory staff and reducing the likelihood of user errors.
7. Quality Control Assurance
Benefit: Built-in quality control functions help monitor and maintain the performance of the analyzer.
Impact: Quality control assurance is crucial for meeting regulatory requirements, ensuring the reliability of results, and maintaining the overall quality of laboratory testing.
8. Cost-Efficiency
Benefit: While initial costs may be higher, the long-term cost efficiency of automatic analyzers is realized through increased throughput and reduced labor costs.
Impact: Laboratories can handle a larger volume of tests with fewer resources, making the overall cost per test more economical.
9. Connectivity and Integration
Benefit: Automatic analyzers often feature connectivity options for integration with laboratory information systems (LIS) and other devices.
Impact: Enhanced connectivity supports seamless data exchange, improving communication between laboratory instruments and facilitating efficient laboratory workflows.
10. Enhanced Patient Care
Benefit: The rapid and accurate results provided by automatic hematology analyzers contribute to timely and precise patient diagnosis and management.
Impact: Improved diagnostic capabilities ultimately lead to enhanced patient care, supporting healthcare professionals in making informed decisions about treatment and intervention.
In summary, the benefits of using automatic hematology analyzers extend beyond efficiency and speed to encompass accuracy, user-friendliness, quality control, and overall cost-efficiency. These instruments play a vital role in modern healthcare by providing reliable and comprehensive hematological information, contributing to better patient outcomes.
Understanding Your Results
Interpreting the results generated by automatic hematology analyzers is a crucial aspect of leveraging these advanced diagnostic tools effectively. Here’s a guide to help you understand the key parameters and values commonly reported in the output of automatic hematology analyzers:
1. Complete Blood Count (CBC)
Parameters: The CBC includes various components such as red blood cell (RBC) count, white blood cell (WBC) count, hemoglobin (Hb) concentration, hematocrit (Hct) level, and platelet count.
Interpretation: Each parameter provides essential information about different aspects of blood health. For example, the RBC count indicates the number of red blood cells, while the WBC count reflects the body’s immune response.
2. Differential White Blood Cell (WBC) Count
Parameters: This part of the CBC breaks down the types of white blood cells, including neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Interpretation: A differential WBC count helps identify specific immune system responses. Abnormalities in the distribution of white blood cell types can provide insights into various medical conditions.
3. Red Blood Cell Indices
Parameters: Mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC).
Interpretation: These indices offer information about the size, hemoglobin content, and concentration of red blood cells. Changes in these values may indicate conditions such as anemia.
4. Platelet Parameters
Parameters: Mean platelet volume (MPV) and platelet distribution width (PDW).
Interpretation: Platelet parameters provide insights into platelet size and distribution, which can be relevant in assessing platelet function and certain disorders.
5. Reticulocyte Count
Parameter: Reticulocyte count reflects the percentage of young, immature red blood cells.
Interpretation: Monitoring reticulocyte count is essential in evaluating bone marrow function and response to anemia treatment.
6. Red Cell Distribution Width (RDW)
Parameter: RDW measures the variation in red blood cell size.
Interpretation: Elevated RDW levels may indicate conditions associated with irregular red blood cell sizes, aiding in the diagnosis of certain blood disorders.
7. Histograms and Scattergrams
Parameters: These visual representations provide a graphical view of cell populations, such as WBC differentials and RBC size distribution.
Interpretation: Histograms and scattergrams offer a more detailed analysis of cell characteristics and can aid in identifying abnormal patterns.
8. Flags and Alerts
Parameters: Automatic hematology analyzers often include flags or alerts for results that fall outside normal ranges.
Interpretation: Pay attention to flags indicating potential issues or abnormalities, and consider further investigation or confirmation tests.
9. Reference Ranges
Parameters: Results are typically accompanied by reference ranges or normal values.
Interpretation: Compare individual results with established reference ranges to determine whether values are within expected limits.
It’s crucial to note that interpretation should be done in the context of the patient’s overall clinical condition, medical history, and other diagnostic information. Additionally, results may vary slightly between different analyzer models and laboratories. Consulting with a healthcare professional is essential for accurate diagnosis and appropriate medical intervention based on the hematology analyzer results.
Conclusion
In conclusion, the realm of automatic hematology analyzers opens a gateway to a deeper understanding of blood health. From the intricacies of blood counts to the applications in healthcare, these analyzers stand as pillars of progress. As you embark on your journey of exploration, remember that this guide is a stepping stone. Encouraging you to delve further, seek additional resources, and, when needed, consult healthcare professionals for personalized advice.
Explore specific diseases, delve into research applications, or simply quench your curiosity. The world of hematology is vast, and your journey within it can be as profound as you choose. As you navigate this path, consider watching a short video demonstrating the basic operation of an automatic hematology analyzer, providing a visual understanding of the technology in action.
Disclaimer
While this guide aims to empower with knowledge, it’s crucial to emphasize that personal health decisions should always be made in consultation with healthcare professionals. The world of blood health is intricate, and expert guidance ensures that the insights gained from automatic hematology analyzers contribute to informed decisions, leading to a healthier, more informed you.
FAQ’s
Why is understanding blood composition crucial in the realm of healthcare, and how do automatic hematology analyzers contribute to this understanding?
Answer: Understanding blood composition is like deciphering the body’s hidden language, and automatic hematology analyzers play a pivotal role in decoding blood counts, providing efficient and precise insights into blood health.
What are the key components and parameters reported by automatic hematology analyzers, and why is understanding them essential for healthcare professionals and individuals?
Answer: Key components include Red Blood Cell (RBC) count, White Blood Cell (WBC) count, Hemoglobin concentration, Hematocrit level, Platelet count, Mean Corpuscular Volume (MCV), and more. Understanding these is crucial for diagnosing conditions like anemia and infections.
How do automatic hematology analyzers work, and what technological advancements do they bring compared to traditional manual blood cell analysis?
Answer: These analyzers use optical and electrical methods to categorize and count blood cells swiftly, automating the process for efficiency and accuracy, overcoming limitations and human errors associated with manual analysis.
What are the key features of automatic hematology analyzers, and how do they contribute to the efficiency and accuracy of laboratory workflows?
Answer: Features include high throughput, precision, comprehensive blood analysis, user-friendly interfaces, sample handling automation, data management, and connectivity. They contribute by processing large sample volumes efficiently, ensuring accurate measurements, and simplifying user interaction.
How do automatic hematology analyzers benefit clinical laboratories and healthcare settings in terms of efficiency, accuracy, and overall cost-effectiveness?
Answer: They streamline blood analysis, providing rapid results and a comprehensive CBC. Their accuracy, reduced manual intervention, advanced data management, and connectivity contribute to overall efficiency, leading to cost-effective operation in the long run.
What are the specific applications and features of automatic hematology analyzers, and how do they contribute to the diagnosis and monitoring of various medical conditions?
Answer: Applications include CBC, differential WBC count, hemoglobin measurement, platelet count and morphology analysis, reticulocyte analysis, and more. These features contribute to the detailed assessment of blood health and aid in diagnosing conditions such as anemia, infections, and blood disorders.
How do automatic hematology analyzers interpret and present results, and what parameters should individuals pay attention to for a better understanding of their blood health?
Answer: Results include CBC parameters, differential WBC counts, red blood cell indices, platelet parameters, reticulocyte count, RDW, histograms, scattergrams, flags, alerts, and reference ranges. Individuals should pay attention to these parameters in the context of their overall health and consult healthcare professionals for interpretation.
What benefits do automatic hematology analyzers offer in terms of efficiency, accuracy, reduced manual intervention, data management, and user-friendliness?
Answer: Benefits include streamlined processes, rapid and high-throughput results, comprehensive analyses, reliability, reduced errors, efficient data management, user-friendly interfaces, and overall cost-efficiency.
How do automatic hematology analyzers contribute to enhanced patient care, and what role do they play in supporting healthcare professionals’ decision-making processes?
Answer: They provide rapid, accurate results, supporting timely diagnosis and treatment decisions. The comprehensive analyses contribute to better patient care, and the efficiency of these analyzers aids healthcare professionals in making informed decisions.
What is the importance of consulting healthcare professionals for result interpretation from automatic hematology analyzers, and how should individuals approach the insights gained from their blood analysis?
Answer: Consulting healthcare professionals is crucial for accurate interpretation based on the individual’s clinical condition and medical history. Individuals should approach the insights gained with a context-aware mindset, understanding that expert guidance ensures informed decisions and contributes to a healthier, more informed lifestyle.




