Picture a labor and delivery room, where a dedicated healthcare team is focused on ensuring the well-being of both the expectant mother and the unborn child. In this critical setting, accurate fetal heart rate monitoring becomes paramount. Imagine a scenario where the precision of this monitoring can make all the difference. Enter Internal Fetal Heart Monitoring (IFHM), a vital tool in the hands of healthcare professionals during labor. This handbook aims to be your comprehensive guide on IFHM, offering insights and guidance to healthcare professionals navigating the intricacies of fetal well-being assessment in the dynamic environment of labor and delivery.
Table of Contents
Brief Explanation of Fetal Heart Monitoring
Fetal heart monitoring involves tracking the baby’s heart rate to ensure it remains within a healthy range during the labor process. This real-time assessment allows healthcare providers to promptly address any signs of distress and make informed decisions to safeguard both maternal and fetal well-being.
Limitations of External FHM Techniques: Doppler Ultrasound Challenges
While external techniques, such as Doppler ultrasound, are commonly used for FHM, they come with limitations. Factors like maternal obesity, suboptimal positioning, and interference from ambient noise can affect the accuracy of readings. Additionally, Doppler ultrasound provides intermittent rather than continuous monitoring, potentially missing critical changes in fetal heart rate patterns.
Introducing Internal Fetal Heart Monitoring (IFHM)
Internal Fetal Heart Monitoring (IFHM) involves placing a fetal scalp electrode on the baby’s scalp to directly measure the heart rate. This method offers a more accurate and continuous assessment compared to external techniques. IFHM provides healthcare professionals with a clearer picture of fetal heart rate patterns, enabling timely interventions when needed.
While external FHM techniques serve as valuable tools, understanding their limitations prompts consideration of more precise methods like IFHM, especially in situations where continuous and accurate monitoring is crucial. As healthcare professionals navigate the complexities of labor care, the choice of fetal heart monitoring techniques plays a pivotal role in ensuring the safety and well-being of both mother and baby.
Also read: A Deep Dive into Fetal Scalp Monitoring in Delivery Supervision
Demystifying Internal Fetal Heart Monitoring (IFHM)
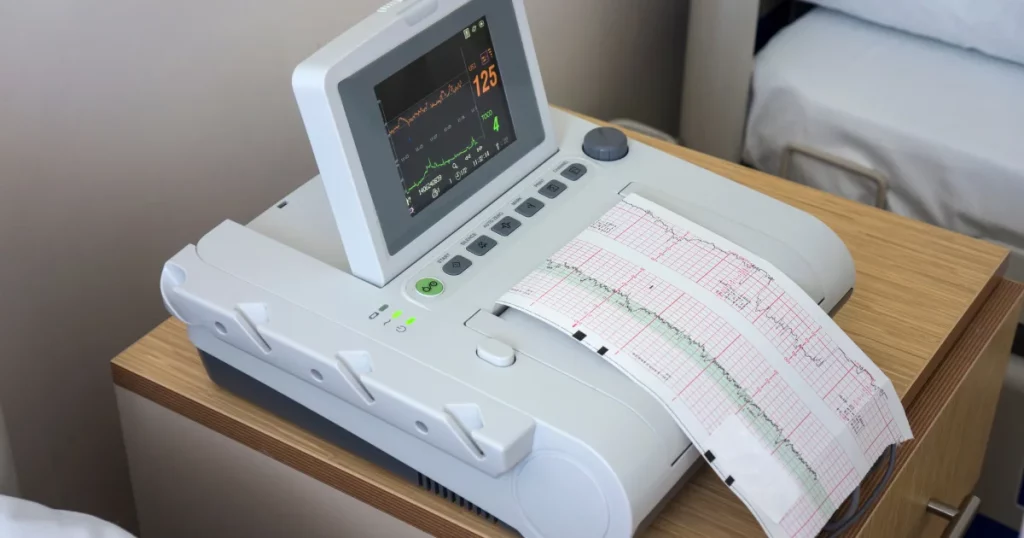
Internal Fetal Heart Monitoring involves directly assessing the fetal heart rate from the baby’s scalp. This intricate system comprises an internal electrode, a connecting cable, and a monitoring device. The magic happens as electrical signals from the fetus translate into visual tracings, offering an accurate representation of the baby’s heartbeat.
Purpose of IFHM
IFHM, or Internal Fetal Heart Monitoring, serves a crucial role in labor and delivery by providing direct and continuous monitoring of the baby’s heart rate. This method offers a more accurate assessment compared to external techniques, allowing healthcare professionals to promptly address any signs of distress during the birthing process.
Components of the IFHM System
The IFHM system comprises three main components:
1. Internal Electrode: A small electrode is gently placed on the baby’s scalp, allowing for the direct measurement of the fetal heart rate. This placement ensures a more reliable and continuous signal compared to external methods.
2. Connecting Cable: The electrode is connected to the monitor through a cable. This cable serves as the conduit for transmitting the electrical signals from the fetus to the monitoring device.
3. Monitor: The monitor displays visual tracings of the fetal heart rate, providing real-time information to healthcare professionals. These tracings help in assessing the baby’s well-being and making informed decisions during labor.
Working Principle of IFHM
The working principle of IFHM involves the translation of electrical signals generated by the fetal heart into visual tracings on the monitor. The internal electrode detects the electrical activity of the baby’s heart, and this information is transmitted through the connecting cable to the monitor. The monitor then displays a continuous and accurate representation of the fetal heart rate patterns, allowing healthcare providers to closely monitor and respond to any changes in real time.
In essence, IFHM offers a direct line of communication with the baby’s heartbeat, providing healthcare professionals with a clearer and more immediate understanding of the fetal heart rate during labor. This precision is especially crucial in situations where continuous monitoring is essential for ensuring the well-being of both the mother and the baby.
When is Internal Fetal Heart Monitor (IFHM) Indicated?

Internal Fetal Heart Monitoring (IFHM) is typically employed in specific situations where a more detailed and direct assessment of the fetal heart rate is warranted. Healthcare professionals may choose IFHM in the following scenarios:
1. High-Risk Pregnancies
High-risk pregnancies with complications that may impact fetal well-being often necessitate closer and more accurate monitoring. IFHM allows for continuous assessment in these critical situations.
2. Non-Reassuring External Monitoring Results
- Decreased Variability: If external monitoring, such as Doppler ultrasound or external tocodynamometry, shows decreased variability in the fetal heart rate, indicating potential issues, healthcare providers may opt for IFHM to obtain a more precise reading.
- Decelerations in Fetal Heart Rate: Patterns of decelerations observed during external monitoring may lead to a decision to switch to IFHM for more accurate and immediate feedback on the baby’s well-being.
3. Suspected Fetal Compromise Based on Clinical Signs
In situations where clinical signs, such as abnormal labor progression or concerns about fetal oxygenation, indicate possible fetal compromise, IFHM becomes a valuable tool. It provides a direct and continuous assessment, allowing for timely intervention.
In these instances, the use of Internal Fetal Heart Monitoring enhances the ability of healthcare professionals to closely monitor and respond to the dynamic conditions of labor, ensuring the safety and well-being of both the mother and the baby. The decision to employ IFHM is made based on careful consideration of the specific circumstances and the need for precise and continuous fetal heart rate evaluation.
How Is an Internal Fetal Monitor Attached?
Internal Fetal Heart Monitoring (IFHM) is a specialized procedure that involves the direct placement of an electrode on the fetal scalp for continuous heart rate monitoring. The following is a step-by-step explanation of the IFHM placement procedure:
1. Informed Consent
Before the procedure, healthcare professionals obtain informed consent from the expectant mother. This involves explaining the purpose of internal fetal monitoring, the procedure itself, and any associated risks or discomfort.
2. Aseptic Preparation
The healthcare provider ensures a sterile environment by washing their hands thoroughly and using aseptic techniques. Sterile gloves are worn to minimize the risk of infection.
3. Positioning
The mother is typically positioned on her back, similar to a pelvic exam. Stirrups may be used for comfort, and the healthcare provider ensures proper exposure while maintaining the patient’s dignity.
4. Vaginal Examination
A vaginal examination is performed to assess the cervix’s dilation and position. This helps determine the feasibility of attaching the internal fetal monitor.
5. Electrode Placement
The internal fetal monitor consists of a small electrode that is attached directly to the baby’s scalp. Using a thin, sterile electrode attached to a wire, the healthcare provider gently inserts the electrode through the cervix and places it on the fetal scalp.
6. Securing the Electrode
Once the electrode is in place, it is secured to the baby’s scalp. The healthcare provider ensures that the connection is stable to obtain accurate and continuous readings.
7. Cable Connection
The wire connected to the electrode is carefully threaded out of the vagina. This cable is then connected to the monitoring device, which displays the fetal heart rate and other relevant information.
8. Comfort and Support
Throughout the process, the healthcare provider communicates with the mother to address any discomfort and provide emotional support. Adequate support is crucial for the overall well-being of the patient.
The internal fetal monitor allows for more precise and continuous monitoring of the baby’s heart rate during labor, especially in situations where external monitoring may be challenging. It’s important to note that this procedure is performed by trained healthcare professionals, and the safety and comfort of both the mother and the baby are prioritized throughout the process.
Interpretation of Internal Fetal Heart Monitoring (IFHM) Tracings
Interpreting IFHM tracings is a crucial aspect of assessing fetal well-being during labor. Here are the basic principles for understanding IFHM tracings:
1. Baseline Heart Rate: The baseline heart rate represents the average fetal heart rate over a 10-minute window. It serves as a reference point for identifying deviations and changes in the fetal heart rate pattern.
2. Variability: Variability refers to the fluctuations in the fetal heart rate around the baseline. Normal variability is a positive sign, indicating a responsive and healthy fetal nervous system. Reduced variability may warrant closer attention.
3. Accelerations and Decelerations: Accelerations are brief increases in the fetal heart rate, often associated with fetal movement. They are considered reassuring signs. On the other hand, decelerations, which are temporary decreases in heart rate, can be categorized as early, late, or variable, and their patterns are crucial in assessing fetal well-being.
4. Recognizing Patterns Suggestive of Fetal Distress: Patterns suggestive of fetal distress may include persistent late decelerations, reduced or absent variability, and prolonged decelerations. These patterns may indicate inadequate oxygenation to the fetus and require prompt evaluation and intervention.
5. Correlating Tracings with Clinical Findings: The interpretation of IFHM tracings should always be correlated with clinical findings. Information about the mother’s medical history, medication use, and responses to interventions complements the tracings, providing a comprehensive understanding of the fetal condition.
Healthcare professionals use their expertise to analyze these elements collectively, making informed decisions about the need for further assessments or interventions. Clear communication with the healthcare team and the patient ensures that the interpretation aligns with the overall clinical context, contributing to optimal care for both the mother and the baby.
Benefits and Risks of Internal Fetal Heart Monitoring (IFHM)

A. Advantages of IFHM
1. Enhanced Detection of Fetal Distress: IFHM provides a more direct and accurate assessment of fetal heart rate, enabling the early detection of signs of distress. This timely information allows healthcare professionals to intervene promptly and optimize outcomes for both mother and baby.
2. Improved Accuracy Compared to External Monitoring: The proximity of the internal electrode to the fetal scalp enhances the accuracy of heart rate recordings. This is especially beneficial in situations where external monitoring might be challenging or when a more precise assessment is required.
3. Potential for Avoiding Unnecessary Cesarean Deliveries: The detailed and accurate information provided by IFHM can contribute to informed decision-making. This may help healthcare professionals avoid unnecessary cesarean deliveries by providing a clearer understanding of the fetal condition.
B. Consideration of Potential Risks and Complications
1. Infection, Bleeding, Discomfort for the Mother: As with any invasive procedure, there is a slight risk of infection, bleeding, or discomfort associated with the insertion of the internal electrode. Healthcare providers take measures to minimize these risks through aseptic techniques and careful monitoring.
2. Fetal Scalp Injury (Rare): While rare, there is a minimal risk of fetal scalp injury during the insertion of the electrode. Healthcare professionals undergo specific training to minimize such risks and prioritize the safety of both the mother and the baby.
In summary, while IFHM offers significant advantages in terms of accuracy and early detection of fetal distress, healthcare providers carefully weigh these benefits against potential risks. The decision to use IFHM is individualized, taking into account the specific circumstances of each pregnancy and the overall well-being of both the mother and the baby. Open communication between healthcare providers and expectant mothers ensures informed decision-making and optimal care throughout the labor process.
Optimizing Internal Fetal Heart Monitoring (IFHM) Usage
Effective utilization of IFHM is crucial for maximizing its benefits and ensuring the safety of both mother and baby. Here are key best practices:
1. Proper Training for Healthcare Professionals
Healthcare professionals involved in IFHM procedures should undergo comprehensive training. This includes hands-on experience in electrode placement, interpretation of tracings, and addressing potential complications. Regular updates and continuing education contribute to maintaining proficiency.
2. Clear Protocols Based on Clinical Guidelines
Establishing clear and evidence-based protocols for the use of IFHM is essential. These protocols should align with clinical guidelines and take into account factors such as gestational age, maternal health, and fetal conditions. Standardized protocols contribute to consistent and reliable monitoring practices.
3. Importance of Clear Communication with the Patient
Prior to IFHM placement, healthcare providers should engage in clear and transparent communication with the patient. This includes explaining the procedure, discussing its purpose, and highlighting the potential benefits and risks. Ensuring that the patient provides informed consent is fundamental to ethical and patient-centered care.
4. Ensuring Informed Consent
Obtaining informed consent is a critical step in the IFHM process. Healthcare providers should ensure that the patient fully understands the procedure, its purpose, and any associated risks. This involves providing information in a clear and understandable manner and addressing any questions or concerns the patient may have.
5. Continuous Monitoring and Evaluation
Throughout the labor process, continuous monitoring and evaluation of both the mother and the baby are essential. Healthcare professionals should closely observe IFHM tracings, correlate them with clinical findings, and intervene promptly if signs of distress are detected.
By adhering to these best practices, healthcare professionals can optimize the usage of IFHM, contributing to improved outcomes for expectant mothers and their babies. Clear communication, ongoing training, and adherence to established protocols are key components of providing safe and effective care during labor and delivery.
Troubleshooting Common Internal Fetal Heart Monitor Issues
Internal Fetal Heart Monitoring (IFHM) is a valuable technique, but like any medical procedure, it may encounter occasional issues. Here’s a guide to troubleshooting common problems:
1. Electrode Displacement
Issue: If the electrode becomes displaced, it can lead to inaccurate readings.
Troubleshooting:
– Ensure that the electrode is securely placed on the fetal scalp during the initial placement.
– Regularly check and adjust the position if necessary, especially during contractions or movements.
2. Unclear Tracings
Issue: Unclear or inconsistent tracings can make interpretation challenging.
Troubleshooting:
– Verify that the electrode is making proper contact with the fetal scalp, ensuring a stable signal.
– Assess and address any maternal movements or contractions that might interfere with the readings.
3. Signal Loss
Issue: Sudden loss of the fetal heart rate signal.
Troubleshooting:
– Inspect the cable and connections for any signs of damage or disconnection.
– Reposition the electrode if needed, ensuring a secure connection.
4. Maternal Discomfort
Issue: Maternal discomfort or pain associated with the internal electrode.
Troubleshooting:
– Communicate effectively with the patient, ensuring they are informed about the procedure and can express any discomfort.
– Consider adjusting the position of the electrode or providing additional support if needed.
5. Infection Concerns
Issue: Risk of infection at the site of electrode placement.
Troubleshooting:
– Adhere strictly to aseptic techniques during placement.
– Monitor the site for signs of infection and promptly address any concerns.
6. Interference from Other Devices
Issue: External devices causing interference with the monitor signal.
Troubleshooting:
– Identify and relocate any electronic devices or equipment that may be causing interference.
– Ensure a clear pathway for the monitor signal.
7. Communication Challenges
Issue: Ineffective communication between healthcare professionals and the patient.
Troubleshooting:
– Prioritize clear and transparent communication, addressing any concerns or questions from the patient.
– Provide ongoing education to healthcare professionals to enhance communication skills.
Remember, if troubleshooting doesn’t resolve the issue, consult with experienced healthcare professionals, and consider involving a specialist in fetal monitoring. The safety and well-being of both the mother and the baby are paramount, and timely resolution of issues ensures accurate monitoring throughout labor.
Internal Fetal Heart Monitoring: Nursing Considerations
Internal fetal heart monitoring (IFHM) is a crucial aspect of labor and delivery care, providing detailed information about the baby’s well-being during the birthing process. Here are key nursing considerations when implementing internal fetal heart monitoring:
1. Informed Consent: Obtain informed consent from the expectant mother before initiating IFHM. Clearly explain the purpose, procedure, potential risks, and benefits to ensure the mother’s understanding and cooperation.
2. Patient Education: Educate the mother about the necessity and benefits of IFHM. Address any concerns or questions she may have, fostering open communication and trust between the healthcare team and the patient.
3. Comfort and Privacy: Prioritize the patient’s comfort and privacy throughout the procedure. Maintain a supportive and reassuring environment to alleviate any anxiety the mother may experience.
4. Sterile Technique: Ensure strict adherence to sterile techniques during the placement of the internal fetal monitor. This helps minimize the risk of infection for both the mother and the baby.
5. Continuous Monitoring: Monitor the baby’s heart rate continuously and observe for any deviations from the normal baseline. Promptly report any concerning patterns to the healthcare provider for further assessment.
6. Positioning: Assist with the appropriate positioning of the mother for the procedure. Offer comfort measures, such as pillows or adjustments, to enhance the mother’s experience during IFHM.
7. Assessment of Fetal Scalp: Collaborate with the healthcare provider in assessing the fetal scalp during the procedure. Ensure proper placement of the electrode on the baby’s scalp for accurate readings.
8. Documentation: Maintain thorough and accurate documentation of the IFHM procedure, including the time of initiation, the baseline fetal heart rate, and any notable changes. Document the mother’s response and any interventions provided.
9. Monitoring for Complications: Be vigilant for potential complications, such as signs of infection or bleeding. Monitor the mother’s vital signs and assess the fetal heart rate for signs of distress.
10. Emotional Support: Provide emotional support to the mother throughout the IFHM process. Address any emotional or psychological aspects related to continuous monitoring and childbirth.
11. Collaboration with the Healthcare Team: Foster effective communication and collaboration with other members of the healthcare team, including obstetricians, midwives, and other nursing staff. Ensure a cohesive approach to patient care.
By incorporating these nursing considerations, healthcare professionals can enhance the safety, comfort, and overall experience of expectant mothers undergoing internal fetal heart monitoring. Patient-centered care and effective communication contribute to a positive birthing experience.
Conclusion
In conclusion, Internal Fetal Heart Monitoring (IFHM) emerges as a valuable tool in obstetric care, offering enhanced precision in assessing fetal well-being during labor. The key takeaways include:
Uses and Benefits
– IFHM is indicated in high-risk pregnancies and situations where external monitoring may be insufficient.
– It provides a more accurate and direct measurement of fetal heart rate, allowing for timely detection of distress.
– The benefits extend to improved outcomes by enabling healthcare professionals to make informed decisions and interventions during labor.
Risks and Considerations
– While IFHM presents advantages, it’s essential to acknowledge potential risks such as infection, bleeding, and discomfort for the mother.
– Fetal scalp injury, though rare, is a consideration, highlighting the importance of skilled placement.
Proper Implementation
– Optimizing the use of IFHM involves proper training for healthcare professionals, clear protocols based on clinical guidelines, and transparent communication with patients.
– Ongoing education is pivotal, ensuring that healthcare providers stay abreast of advancements and maintain proficiency in IFHM procedures.
Improving Outcomes in High-Risk Pregnancies
– IFHM plays a crucial role in improving outcomes for pregnancies deemed high-risk, offering a higher level of fetal monitoring precision.
– Timely detection of distress allows for prompt interventions, potentially reducing the need for unnecessary cesarean deliveries.
As the field of obstetrics evolves, a commitment to best practices, continuous education, and adherence to established protocols ensures that IFHM remains a reliable and effective tool in safeguarding the health and well-being of both mothers and their newborns.