Urine analysis is a cornerstone in medical diagnostics, offering insights into various health aspects. This comprehensive guide navigates through the spectrum of urine analyzers, covering everything from traditional dipsticks to advanced laboratory technologies.
Table of Contents
Dipstick Urinalysis
Dipstick urinalysis is a rapid and common diagnostic test that provides valuable insights into an individual’s health by examining the chemical composition of their urine. This non-invasive method utilizes a chemically treated strip, commonly known as a dipstick, to assess various parameters. Here’s a comprehensive look at the significance, procedure, and interpretation of dipstick urinalysis:

1. Purpose and Significance
- Diagnostic Tool: Dipstick urinalysis serves as a diagnostic tool to evaluate renal and metabolic health, screen for potential infections, and monitor certain medical conditions.
- Routine Screening: It is commonly employed in routine health check-ups, prenatal care, and the management of chronic diseases such as diabetes and kidney disorders.
2. Parameters Examined
- pH Level: Indicates the acidity or alkalinity of the urine, providing insights into metabolic processes.
- Protein: Elevated levels may suggest kidney dysfunction or other underlying conditions.
- Glucose: Abnormal levels may be indicative of diabetes or other metabolic disorders.
- Ketones: Presence may signal the breakdown of fats, often seen in diabetes or fasting.
- Blood: Detects blood in the urine, which may result from various conditions, including infections or kidney stones.
- Nitrites: Presence may indicate a urinary tract infection.
- Leukocytes: Elevated levels suggest inflammation or infection in the urinary tract.
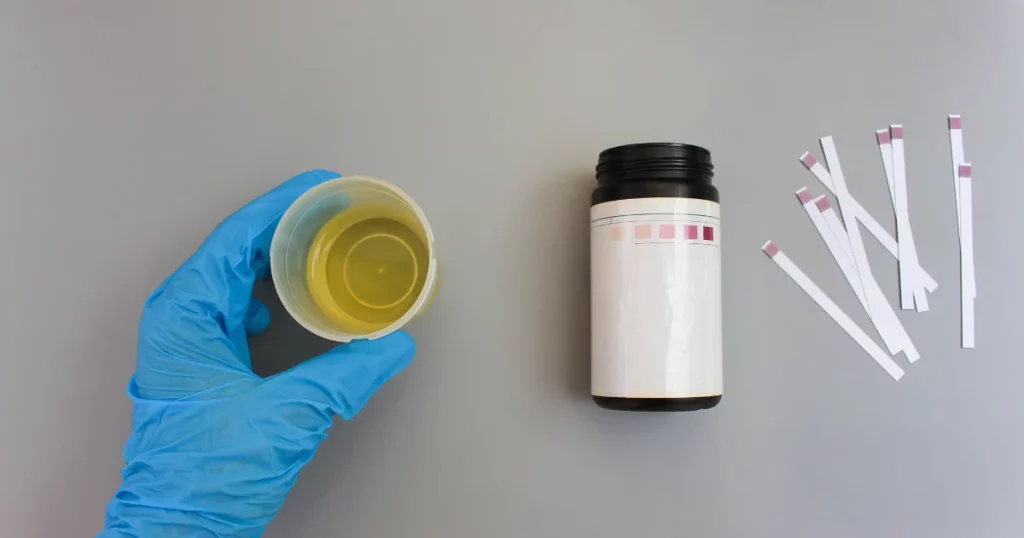
3. Procedure
- Sample Collection: A fresh urine sample is collected in a clean container, usually midstream to minimize contaminants.
- Dipstick Immersion: The dipstick is dipped into the urine sample for a specified time, allowing the chemical reactions to occur.
- Color Changes: Chemical reactions on the dipstick lead to color changes, which are then compared to a color chart provided by the manufacturer.
4. Interpretation of Results
- Color Matching: Results are interpreted by comparing the color changes on the dipstick to the reference colors on the chart.
- Normal vs. Abnormal: Deviations from the normal range in any parameter may suggest underlying health issues, prompting further investigation.
5. Limitations and Considerations
- False Positives/Negatives: Certain medications or dietary factors can influence results, leading to false readings.
- Complementary Testing: Dipstick urinalysis is often complemented by additional tests, such as microscopic examination, for a more comprehensive assessment.
6. Clinical Applications
- Disease Monitoring: Regular dipstick urinalysis aids in monitoring chronic conditions like diabetes or kidney diseases.
- Infection Detection: It is valuable in identifying urinary tract infections or conditions associated with hematuria.
7. Professional Guidance
- Healthcare Provider Interpretation: Results should be interpreted by healthcare professionals who consider the patient’s medical history and other relevant factors.
- Follow-Up Tests: Abnormal findings may warrant further diagnostic tests to confirm and understand the underlying cause.
Dipstick urinalysis, with its simplicity and speed, plays a pivotal role in the initial assessment of urinary health. While it offers valuable insights, its results are most effectively interpreted within the context of a broader clinical evaluation by healthcare professionals. Regular monitoring through dipstick urinalysis contributes to proactive healthcare, enabling early detection and intervention for various medical conditions.
Explore our best-selling products.
Portable Urine Analyzers
Portable urine analyzers stand at the forefront of diagnostic innovation, offering convenient and efficient tools to analyze urine samples rapidly. These compact devices bring the diagnostic capabilities of a traditional laboratory to the point of care, enabling healthcare professionals to make swift and informed decisions. Let’s delve into the features, benefits, and applications that make portable urine analyzers integral in modern healthcare:
1. Compact Design and Mobility
- On-the-Go Diagnostics: Portable urine analyzers are designed for mobility, allowing healthcare professionals to conduct urine analysis directly at the patient’s bedside or in remote settings.
- Compact Form: Their small size and lightweight design make them easy to carry, ensuring flexibility in various healthcare environments.
2. Automated Analysis
- Efficiency and Speed: These analyzers automate the urine analysis process, delivering results within minutes. This efficiency enhances the speed of diagnosis and enables prompt decision-making in critical situations.
- User-Friendly Operation: Most portable urine analyzers are designed with user-friendly interfaces, requiring minimal training for healthcare professionals to operate effectively.
3. Multifaceted Parameter Analysis
- Comprehensive Testing: Portable urine analyzers are equipped to analyze multiple parameters, including pH, protein, glucose, ketones, and more.
- Broad Clinical Insight: The ability to assess various parameters provides a comprehensive overview of a patient’s urinary health, aiding in the diagnosis of conditions such as diabetes, kidney disorders, and urinary tract infections.
4. Point-of-Care Diagnostics
- Immediate Results: The point-of-care nature of these analyzers means that healthcare professionals can obtain immediate results, allowing for timely intervention and treatment planning.
- Reduced Turnaround Time: Eliminating the need for sample transportation to a centralized laboratory reduces the overall turnaround time for diagnostic information.
5. Data Connectivity
- Integration with Information Systems:* Many portable urine analyzers are designed to seamlessly integrate with healthcare information systems, facilitating electronic record-keeping and data sharing.
- Enhanced Workflow: Connectivity features contribute to a streamlined workflow, ensuring that diagnostic information is readily available to healthcare teams.
6. Infection Control Measures
- Disposable Components: Some portable urine analyzers utilize disposable components, minimizing the risk of cross-contamination between samples.
- Hygienic Operation: This feature enhances infection control measures, particularly in settings where rapid and repeated testing is essential.
7. Applications Across Healthcare Settings
- Primary Care: Portable urine analyzers find applications in primary care settings for routine health check-ups, allowing for quick and routine urinary assessments.
- Emergency Departments: In emergency situations, these analyzers provide rapid insights, aiding in the triage and immediate management of patients.
- Remote Healthcare: In remote or resource-limited settings, portable urine analyzers serve as invaluable tools for basic diagnostic assessments.
8. Quality Assurance and Calibration
- Regular Calibration: Manufacturers often provide calibration options, ensuring the accuracy and reliability of results.
- Quality Assurance: Regular maintenance and calibration contribute to the longevity and performance of these analyzers.
9. Cost-effective and Resource-Efficient
- Reduced Costs: Portable urine analyzers can contribute to cost savings by eliminating the need for external laboratory services, especially in situations where frequent testing is required.
- Resource Efficiency: Their efficiency and speed contribute to resource optimization, making them economically viable for healthcare facilities.
Portable urine analyzers represent a paradigm shift in point-of-care diagnostics, aligning with the evolving needs of modern healthcare. Their ability to provide rapid, accurate, and comprehensive urine analysis fosters timely clinical decision-making, ultimately enhancing patient care. As technological advancements continue, these portable analyzers are likely to play an increasingly pivotal role in diagnostic workflows, offering convenience without compromising on the quality of results.
Semi-Automated Analyzers
Semi-automated urine analyzers stand as essential tools in clinical laboratories, seamlessly blending automation with human oversight. These analyzers streamline the urine testing process, offering a middle ground between manual methods and fully automated systems. Let’s explore the distinctive features, advantages, and applications that position semi-automated urine analyzers as key players in diagnostic workflows:
1. Semi-Automation for Efficiency
- Strategic Balance: Semi-automated analyzers strike a balance between manual techniques and fully automated systems. They automate specific aspects of urine analysis while retaining a degree of manual intervention for tasks requiring human judgment.
- Time Efficiency: By automating routine tasks, these analyzers significantly reduce the time and effort required for urine sample processing, contributing to overall laboratory efficiency.
2. User-Friendly Operation
- Ease of Use: Semi-automated analyzers are designed with user-friendly interfaces, ensuring that laboratory technicians can operate them with minimal training.
- Flexibility: Technicians retain control over certain steps of the analysis, allowing for flexibility in handling diverse sample types and addressing specific testing requirements.
3. Parameter Variety
- Multiple Analyte Testing: These analyzers can assess a range of parameters, including pH, protein, glucose, and more. The ability to analyze multiple analytes in a single run provides a comprehensive view of a patient’s urinary health.
- Diagnostic Insights: The diversity of parameters covered enhances diagnostic capabilities, aiding in the identification of various conditions such as kidney disorders and urinary tract infections.
4. Quality Assurance Measures
- Internal Quality Controls: Semi-automated analyzers often incorporate internal quality control features to monitor and ensure the accuracy and precision of results.
- Calibration Options: Laboratories can calibrate these analyzers regularly to maintain the reliability of diagnostic outcomes.
5. Workflow Integration
- Integration Capabilities: Semi-automated urine analyzers seamlessly integrate with laboratory information systems, facilitating efficient data management and reporting.
- Enhanced Workflow: The integration of these analyzers into laboratory workflows contributes to a streamlined and organized diagnostic process.
6. Laboratory Standardization
- Consistency: Semi-automated analyzers contribute to standardization in laboratory procedures, ensuring consistent testing practices.
- Reduced Variability: By automating certain steps, these analyzers help minimize variability introduced by manual techniques, leading to more reliable results.
7. Applications Across Laboratory Settings
- Medium to High-Volume Laboratories: Semi-automated analyzers are well-suited for laboratories with moderate to high testing volumes, offering efficiency without the full automation scale.
- Routine Screening: Their capabilities make them suitable for routine urine screening, allowing laboratories to handle a significant number of samples daily.
8. Cost-Effective Solution
- Optimized Resources: Semi-automated analyzers provide a cost-effective solution for laboratories seeking increased efficiency without the expense of fully automated systems.
- Resource Allocation: Laboratories can allocate resources effectively, balancing automation benefits with manual oversight.
Semi-automated urine analyzers embody a versatile approach to urine analysis, catering to the needs of laboratories aiming for efficiency and diagnostic precision. Their ability to combine automation with human control positions them as valuable assets in various clinical settings, contributing to the delivery of accurate and timely diagnostic information for patient care.
Fully Automated Laboratory Systems

Fully automated systems have emerged as transformative forces, particularly in the field of urine analysis. These advanced systems integrate cutting-edge technology to streamline and enhance the entire urinalysis process. Let’s delve into the remarkable features, benefits, and applications that characterize fully automated laboratory systems for urine analysis:
1. Comprehensive Automation
- End-to-End Processing: Fully automated systems cover the entire spectrum of urine analysis, from sample preparation to result reporting.
- Minimized Manual Intervention: These systems significantly reduce the need for manual handling, automating tasks such as sample centrifugation, pipetting, and result interpretation.
2. High Throughput Capabilities
- Efficient Sample Processing: Fully automated systems excel in handling a high volume of urine samples efficiently, making them ideal for laboratories with substantial testing demands.
- Rapid Turnaround: The high throughput capacity ensures swift processing of samples, contributing to quicker diagnostic outcomes.
3. Broad Analytical Parameters
- Extensive Analyte Coverage: These systems can analyze a wide array of parameters, including but not limited to pH, protein, glucose, ketones, and sediment components.
- Holistic Diagnostic Insights: The ability to assess multiple analytes in a single run provides a comprehensive overview of a patient’s urinary health.
4. Precision and Accuracy
- Advanced Calibration and Quality Control: Fully automated systems incorporate sophisticated calibration mechanisms and internal quality control measures to ensure the precision and accuracy of results.
- Minimized Variability: Automation reduces the potential for human error, enhancing the reliability of diagnostic outcomes.
5. User-Friendly Interfaces
- Intuitive Operation: These systems feature user-friendly interfaces, allowing laboratory technicians to operate them with ease.
- Minimal Training Requirements: The streamlined workflow and intuitive design minimize the learning curve, enabling efficient use by laboratory staff.
6. Connectivity and Integration
- Seamless Data Management: Fully automated systems seamlessly integrate with laboratory information systems, facilitating efficient data management and reporting.
- Enhanced Workflow Integration: The connectivity ensures smooth communication between different components of the laboratory, optimizing overall workflow.
7. Customization and Flexibility
- Adaptable to Testing Needs: Laboratories can customize the testing panels based on specific diagnostic requirements.
- Flexibility in Sample Types: Fully automated systems can handle various sample types, accommodating the diversity of patient specimens.
8. Laboratory Standardization
- Consistency in Results: The automation of processes contributes to standardization in laboratory procedures, ensuring consistent testing practices.
- Reduced Variability: Fully automated systems minimize variability introduced by manual techniques, leading to reproducible and reliable results.
9. Enhanced Laboratory Efficiency
- Resource Optimization: Fully automated systems optimize laboratory resources by reducing the need for extensive manual labor.
- Time and Cost Savings: The efficient workflow translates into time and cost savings, making these systems a valuable investment for laboratories.
10. Applications Across Diverse Settings
- Large Reference Laboratories: Fully automated systems are particularly suited for high-volume laboratories with diverse testing needs.
- Clinical Settings: Their efficiency makes them valuable in clinical settings where timely and accurate diagnostic information is crucial for patient care.
Fully automated laboratory systems for urine analysis represent a pinnacle of technological advancement in diagnostics. Their ability to combine precision, speed, and adaptability positions them as indispensable tools for modern laboratories, contributing to the delivery of reliable and efficient urinalysis results for enhanced patient care.
Parameters Analyzed by Urine Analyzers
Urine analyzers are sophisticated diagnostic instruments designed to unravel a wealth of information about an individual’s health through the analysis of various parameters. These parameters offer crucial insights into renal function, metabolic status, and potential health concerns. Let’s explore the key parameters analyzed by urine analyzers:
1. pH Level
- Definition: pH reflects the acidity or alkalinity of urine.
- Clinical Significance: Altered pH levels may indicate metabolic imbalances or kidney dysfunction.
2. Protein
- Definition: The presence of protein in urine, known as proteinuria, can be an early sign of kidney disease.
- Clinical Significance: Detecting abnormal protein levels aids in identifying renal issues.
3. Glucose
- Definition: The measurement of glucose in urine indicates the potential presence of diabetes or other metabolic disorders.
- Clinical Significance: Monitoring glucose levels helps in diabetes management and early detection of related complications.
4. Ketones
- Definition: The presence of ketones may suggest abnormal fat metabolism.
- Clinical Significance: Elevated ketone levels are associated with conditions such as diabetic ketoacidosis.
5. Bilirubin
- Definition: Bilirubin in urine may indicate liver dysfunction or hemolysis.
- Clinical Significance: Detecting bilirubin helps assess liver health and identify certain types of anemia.
6. Blood
- Definition: The presence of blood in urine may result from various conditions, including urinary tract infections, kidney stones, or trauma.
- Clinical Significance: Identifying blood in urine aids in diagnosing underlying issues affecting the urinary system.
7. Nitrites
- Definition: Nitrites are indicators of bacterial infections in the urinary tract.
- Clinical Significance: Positive nitrite results suggest the presence of bacteria, guiding the diagnosis of urinary tract infections.
8. Leukocytes
- Definition: Elevated leukocyte levels may indicate inflammation or infection.
- Clinical Significance: Monitoring leukocytes helps identify urinary tract infections and other inflammatory conditions.
9. Urobilinogen
- Definition: Urobilinogen is a byproduct of bilirubin breakdown.
- Clinical Significance: Abnormal levels may indicate liver dysfunction or hemolytic disorders.
10. Specific Gravity
- Definition: Specific gravity assesses the concentration of solutes in urine.
- Clinical Significance: Changes in specific gravity may reflect hydration status and renal function.
11. Creatinine
- Definition: Creatinine levels help evaluate kidney function.
- Clinical Significance: Abnormal creatinine levels may suggest impaired renal function.
12. Microscopic Elements (Sediment)
- Definition: Microscopic analysis assesses elements such as red blood cells, white blood cells, crystals, and casts.
- Clinical Significance: Identifying these elements aids in diagnosing specific kidney disorders and urinary tract issues.
Urine analyzers play a pivotal role in deciphering these parameters, providing healthcare professionals with valuable information for accurate diagnosis and effective patient care. The comprehensive analysis of urine allows for the early detection of abnormalities, contributing to proactive management and improved patient outcomes.
Workflow of Automated Systems
Automated systems for urine analyzers have revolutionized the diagnostic process, streamlining the workflow for efficient and accurate results. Understanding the sequential steps in these automated systems offers insights into their functionality:
1. Sample Collection
Automated urine analyzers typically begin with the collection of urine samples, either through manual collection or directly from sample cups.
2. Sample Identification
The automated system utilizes barcode scanning or other identification methods to ensure accurate matching of samples with patient information.
3. Sample Preparation
The urine sample undergoes preparation steps, which may include centrifugation to separate particles, ensuring a homogenous sample for analysis.
4. Automated Dipstick Analysis
Some systems employ automated dipstick analysis, where a robotic arm dips a reagent-embedded strip into the urine sample. The system then captures images and interprets the color changes on the dipstick.
5. Optical Measurement
Advanced automated systems utilize optical measurement techniques for analyzing various parameters. This involves shining light through the urine sample and measuring the absorbance or fluorescence to quantify specific components.
6. Chemical Reaction Detection
Automated analyzers detect chemical reactions occurring in the sample, such as enzymatic reactions for glucose or protein quantification. The system interprets these reactions to determine analyte concentrations.
7. Data Processing
The collected data undergoes sophisticated processing algorithms within the system. This includes converting optical signals into numerical values and interpreting color changes for qualitative assessments.
8. Result Generation
The final results, including numerical values and qualitative interpretations, are generated by the automated system. These results are typically displayed on a computer screen or printed for review by healthcare professionals.
9. Quality Control
Automated systems incorporate built-in quality control measures to ensure the accuracy and reliability of results. This includes regular calibration, verification of reagent integrity, and system checks.
10. Integration with Laboratory Information System (LIS)
Many automated urine analyzers seamlessly integrate with laboratory information systems. This facilitates the electronic storage of results, patient data, and provides a comprehensive record for healthcare professionals.
11. Reporting
The system generates comprehensive reports summarizing the results, often including reference ranges for each parameter. These reports can be easily accessed by healthcare providers for diagnostic and decision-making purposes.
12. Maintenance and Cleaning
Automated systems are designed with maintenance features, including self-cleaning mechanisms and routine maintenance schedules. This ensures the longevity and reliability of the analyzer.
Understanding the workflow of automated systems for urine analyzers highlights the technological advancements that contribute to precision, efficiency, and consistency in diagnostic processes. These automated solutions play a vital role in modern healthcare, enhancing laboratory capabilities and ultimately improving patient care.
Interpretation of Urine Test Results
Interpreting results from urine analyzers is a critical step in extracting meaningful information for diagnostic purposes. The data generated by these analyzers encompass various parameters, each providing insights into the patient’s health. Here’s a guide to understanding and interpreting the results:
1. Urinary pH
Normal Range: Typically, urine pH falls within the range of 4.5 to 8.0.
Interpretation: A pH below 7 indicates acidic urine, while a pH above 7 indicates alkaline urine. Deviations from the normal range may indicate metabolic imbalances or kidney issues.
2. Protein (Proteinuria)
Normal Range: Normally, urine should contain minimal protein.
Interpretation: Elevated protein levels may suggest kidney dysfunction or other underlying conditions. Persistent proteinuria requires further investigation.
3. Glucose (Glycosuria)
Normal Range: Healthy individuals usually have minimal or no glucose in their urine.
Interpretation: Detecting glucose may indicate diabetes or impaired glucose metabolism. Consistent glycosuria warrants glucose tolerance testing.
4. Ketones (Ketonuria)
Normal Range: Ketones are generally absent in urine.
Interpretation: The presence of ketones may indicate conditions such as uncontrolled diabetes, fasting, or ketogenic diets. Further clinical assessment is crucial.
5. Blood (Hematuria)
Normal Range: Healthy urine is typically clear without visible blood.
Interpretation: Hematuria suggests blood in the urine and may be indicative of urinary tract infections, kidney stones, or other urinary system disorders.
6. Bilirubin and Urobilinogen
Normal Range: Bilirubin and urobilinogen are normally present in trace amounts.
Interpretation: Elevated levels may indicate liver disorders or hemolysis. Further investigations, including liver function tests, may be necessary.
7. Nitrites
Normal Range: Nitrites are typically absent in urine.
Interpretation: The presence of nitrites may suggest bacterial infections in the urinary tract. Additional tests, such as urine culture, are often performed for confirmation.
8. Leukocytes (Leukocyturia)
Normal Range: In healthy individuals, leukocytes are not typically present in urine.
Interpretation: Elevated leukocytes may indicate urinary tract infections or inflammation. Additional clinical assessment and urine culture are often recommended.
9. Specific Gravity
Normal Range: Specific gravity ranges from 1.005 to 1.030.
Interpretation: Deviations from the normal range may indicate hydration status. Low specific gravity may suggest dilute urine, while high specific gravity may indicate concentrated urine.
10. Creatinine and Microalbumin
Normal Range: Trace amounts of creatinine and microalbumin are present in urine.
Interpretation: Elevated levels may indicate kidney dysfunction. Microalbuminuria is an early sign of kidney damage and requires further evaluation.
11. Urine Sediment Examination
Microscopic examination of urine sediment provides insights into the presence of cells, crystals, and casts. Abnormal findings may guide further diagnostic investigations.
12. Reference Ranges
It is crucial to compare individual results with established reference ranges provided by the laboratory. Deviations outside these ranges warrant clinical attention.
13. Clinical Correlation
While urine analyzer results provide valuable information, they should be interpreted in the context of the patient’s clinical history, symptoms, and other diagnostic findings.
Understanding the interpretation of results from urine analyzers requires a comprehensive approach, considering various parameters and their interplay. Healthcare professionals play a pivotal role in analyzing these results, correlating them with clinical information, and guiding appropriate interventions for patient care.
Challenges in Urinalysis
Performing urinalysis is a routine yet crucial aspect of diagnostic medicine, providing valuable insights into a patient’s health. However, several challenges may be encountered during the process, requiring careful consideration and expertise. Here are the key challenges in urinalysis:
1. Contamination
- Challenge: External contaminants, such as toilet tissue or soap, can compromise the accuracy of urinalysis results.
- Mitigation: Proper patient education on clean catch techniques and providing suitable collection containers can minimize contamination.
2. Timeliness
- Challenge: For accurate results, fresh urine samples are preferable. Delayed analysis may lead to changes in cellular and chemical components.
- Mitigation: Encouraging prompt sample collection and immediate analysis help maintain result reliability.
3. Temperature Sensitivity
- Challenge: Some analytes, like crystals or cells, can be temperature-sensitive, potentially leading to altered results.
- Mitigation: Analyzing samples promptly after collection and avoiding prolonged exposure to extreme temperatures help maintain stability.
4. Evaporation Effects
- Challenge: Extended exposure to air can lead to the evaporation of water content in the urine, affecting specific gravity and analyte concentrations.
- Mitigation: Sealing sample containers promptly after collection prevents evaporation-related issues.
5. Sample Volume Variability
- Challenge: Inconsistent urine sample volumes may impact the accuracy of results, especially in automated analyzers.
- Mitigation: Providing clear instructions to patients regarding the required sample volume helps standardize the analysis process.
6. Physiological Factors
- Challenge: Factors like hydration status, diet, and medication use can influence urine composition.
- Mitigation: Clinicians must consider these factors during result interpretation and seek additional information from patients when necessary.
7. Interference from Medications
- Challenge: Certain medications can interfere with urinalysis results, affecting parameters like color or chemical composition.
- Mitigation: Obtaining a detailed medication history and communicating potential interferences enhance result accuracy.
8. Urine Storage Conditions
- Challenge: Improper storage conditions, such as exposure to light or inadequate refrigeration, may impact stability.
- Mitigation: Ensuring proper storage according to laboratory guidelines preserves sample integrity.
9. Limited Specificity
- Challenge: Some urinalysis parameters may lack specificity, requiring additional tests for precise diagnostic conclusions.
- Mitigation: Integrating urinalysis results into a broader clinical context helps clinicians make informed decisions.
10. Automated Analyzer Limitations
- Challenge: Automated analyzers may face challenges in distinguishing certain elements, requiring manual confirmation.
- Mitigation: Manual review by laboratory professionals ensures accurate interpretation, especially for complex samples.
Successfully navigating these challenges in urinalysis requires a combination of patient education, laboratory diligence, and clinical expertise. Healthcare professionals play a vital role in addressing these considerations to obtain reliable results for optimal patient care.
Final Words
From the simplicity of dipsticks to the complexity of automated laboratory systems, this guide serves as a roadmap through the diverse world of urine analyzers. Whether you’re a healthcare professional or someone intrigued by medical technology, understanding the nuances of urine analysis is crucial for accurate diagnostics and patient care.