Monitoring fetal heart rate and contractions is a vital aspect of obstetric care, providing insights into the well-being of both the mother and the baby during labor. This guide aims to decode fetal monitor patterns, specifically focusing on understanding contractions. Whether you’re a healthcare professional or an expectant parent, this comprehensive guide offers valuable insights into interpreting fetal monitor patterns for a smoother labor experience.
Table of Contents: Fetal Monitor Patterns
Importance of Fetal Monitoring

Fetal monitoring is a critical aspect of prenatal care that involves tracking the well-being and development of the unborn child throughout pregnancy. This process is essential for various reasons, ensuring the health and safety of both the expectant mother and the fetus:
1. Early Issue Detection: Fetal monitoring enables healthcare professionals to identify potential complications or abnormalities early in pregnancy, allowing for timely interventions and preventive measures.
2. Risk Reduction in High-Risk Pregnancies: In cases of high-risk pregnancies, continuous monitoring provides a vigilant approach to managing conditions such as gestational diabetes, preeclampsia, or other complications, minimizing associated risks.
3. Guiding Delivery Decisions: Monitoring assists healthcare providers in determining the optimal timing and method of delivery, considering factors like gestational age, fetal development, and maternal health.
4. Labor Surveillance: During labor, continuous fetal monitoring helps assess the baby’s response to contractions, aiding in the prompt identification of signs of distress and facilitating timely interventions.
5. Preventing Stillbirths: Regular monitoring plays a crucial role in identifying abnormalities that may pose risks to the unborn child, contributing to the prevention of stillbirths.
6. Multiple Pregnancy Management: In pregnancies involving twins or multiples, vigilant monitoring is particularly important, allowing for personalized care for each baby’s progress and addressing potential challenges.
7. Enhancing Communication: Fetal monitoring fosters open communication between expectant parents and healthcare providers, offering reassurance through visible signs of the baby’s well-being and promoting a positive pregnancy experience.
Also read: Fetal Growth Monitoring
Types of Fetal Monitoring
Fetal monitoring encompasses various techniques to assess the well-being and development of the unborn child during pregnancy. These monitoring methods can be categorized into two main types:
1. External Fetal Monitoring
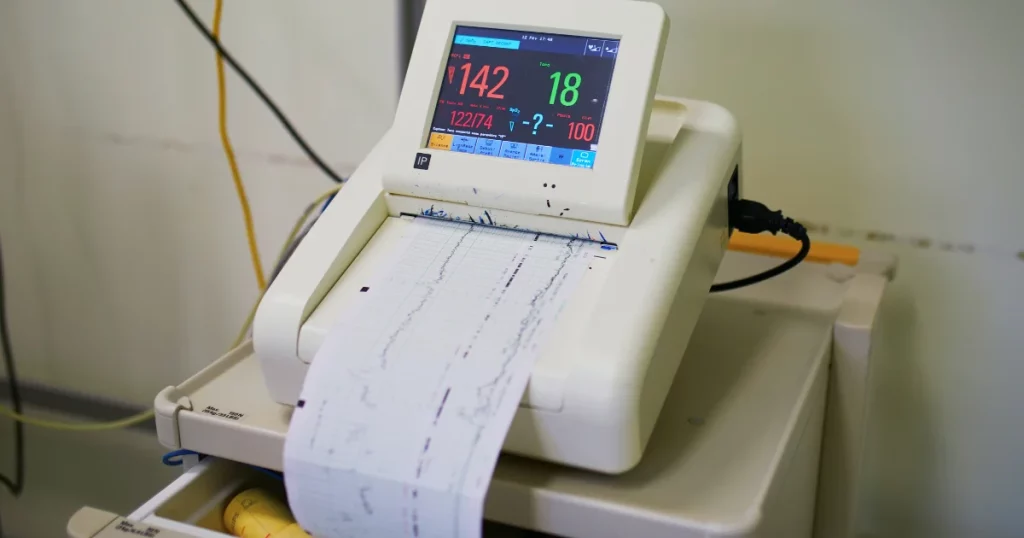
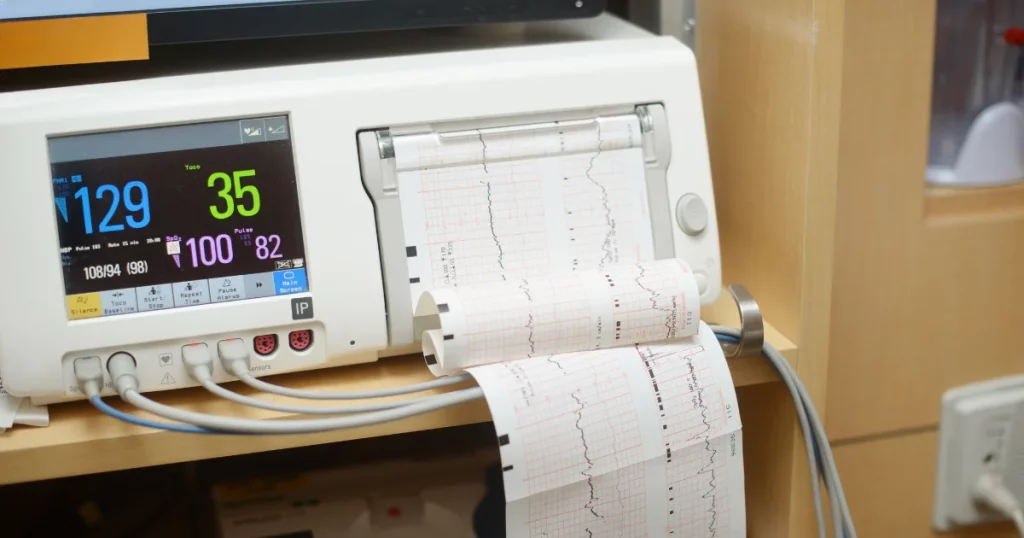
- Doppler Ultrasound: This non-invasive technique uses ultrasound waves to detect and monitor the baby’s heart rate by placing a transducer on the mother’s abdomen. It provides real-time information on fetal well-being.
- External Electronic Fetal Monitoring (EFM): Straps with sensors are placed on the mother’s abdomen to monitor uterine contractions and the baby’s heart rate externally. This method is commonly used during labor to track fetal responses.
2. Internal Fetal Monitoring
- Fetal Scalp Electrode (FSE): In certain situations, a small electrode may be attached to the baby’s scalp through the cervix during labor. This provides more direct and accurate measurements of the fetal heart rate.
- Intrauterine Pressure Catheter (IUPC): This internal monitoring method involves placing a catheter through the cervix into the uterus to measure the strength and frequency of contractions.
The choice between external and internal monitoring depends on factors such as the stage of labor, the need for continuous monitoring, and the specific circumstances of the pregnancy. Each type of monitoring serves a unique purpose in ensuring the safety and well-being of both the mother and the unborn child.
Reading Contractions on the Monitor
Interpreting contractions on a fetal monitor is a crucial aspect of monitoring the progress of labor and ensuring the well-being of both the mother and the baby. Here’s how to read and understand contractions on the fetal monitor:
1. Frequency: This refers to how often contractions occur and is measured in minutes. For example, a frequency of 3 minutes means there are three minutes between the start of one contraction and the start of the next.
2. Duration: Duration indicates how long each contraction lasts and is measured in seconds. A contraction typically lasts between 30 seconds to a minute.
3. Intensity: The strength or intensity of contractions is an essential factor. Fetal monitors often use different scales or patterns to represent contraction strength. A higher intensity may be indicative of effective labor.
4. Resting Tone: The resting tone is the level of tension in the uterine muscle between contractions. It should return to a baseline level during the intervals between contractions.
Understanding these parameters helps healthcare providers assess the progress of labor and make informed decisions about the well-being of the baby. Consistent and effective contractions are essential for the progression of labor and the eventual delivery of a healthy baby. Healthcare professionals closely monitor these factors to ensure a safe and successful childbirth experience.
Understanding Uterine Activity
Understanding uterine activity is a crucial aspect of monitoring the progress of labor. Here are the key components involved in comprehending uterine activity:
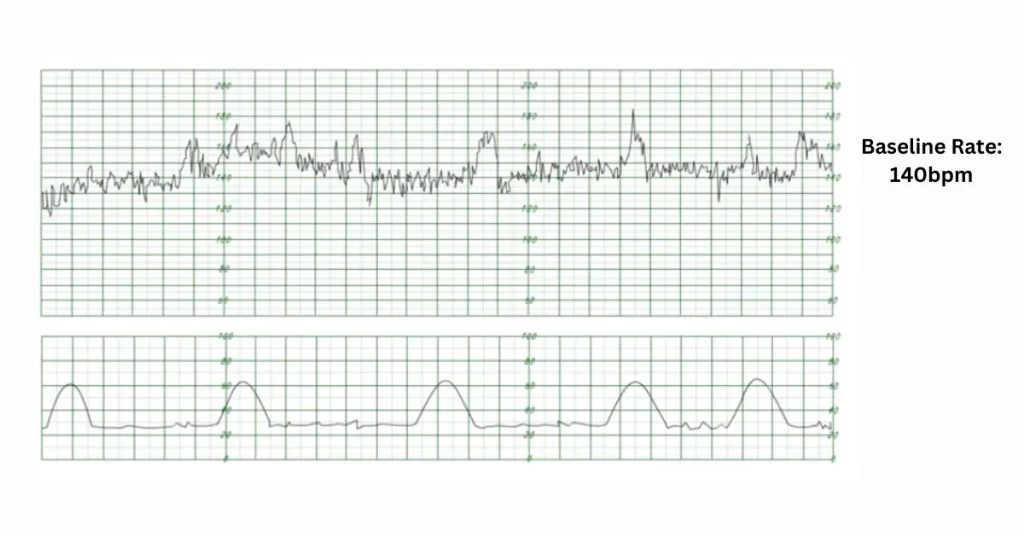
- Contractions on the Tocodynamometer: External monitors utilize a tocodynamometer to display contractions. This device showcases peaks that correspond to each contraction, offering a visual representation of uterine activity.
- Waveform Analysis: Analyzing the waveform pattern is essential for understanding uterine activity. This analysis helps identify the gradual buildup and release of uterine tension during contractions. The waveform provides valuable insights into the characteristics and strength of contractions, aiding healthcare providers in assessing the labor process. This information is instrumental in ensuring the well-being of both the mother and the baby during childbirth.
Differentiating Between True and False Contractions
Distinguishing between true and false contractions is a key aspect of fetal monitoring, ensuring accurate assessment of labor progress. Here’s how to differentiate between these types of contractions:
1. True Contractions (Labor Contractions)
- Regular Pattern: True contractions follow a consistent and regular pattern, increasing in frequency and intensity over time.
- Painful Sensation: True contractions are often associated with pain or discomfort, starting in the lower back and radiating to the front of the abdomen.
2. False Contractions (Braxton Hicks Contractions)
- Irregular Pattern: False contractions, also known as Braxton Hicks contractions, have an irregular pattern and do not follow a specific rhythm.
- Less Painful: While they may cause some discomfort, false contractions are generally less painful than true contractions.
Distinguishing between these types of contractions is essential for healthcare providers to accurately interpret fetal monitor data and provide appropriate care during labor. Regular and painful contractions are indicative of true labor, signaling the progression toward childbirth. In contrast, irregular and less painful contractions are considered false contractions, which are a common occurrence throughout pregnancy but don’t lead to labor.
Patterns Indicating Progress
Monitoring patterns in fetal heart rate and uterine contractions is crucial for assessing the progress of labor. Here are patterns that indicate progress in a fetal monitor:
1. Normal Fetal Heart Rate Patterns
- Baseline Fetal Heart Rate (FHR): A stable baseline heart rate within the normal range (120-160 beats per minute) suggests the well-being of the fetus.
- Variability: A healthy heart rate demonstrates variability, representing the ability of the fetal autonomic nervous system to respond to stimuli.
2. Accelerations
- Rapid Increase in FHR: Accelerations are quick increases in the fetal heart rate, usually in response to fetal movement, indicating a well-oxygenated and responsive baby.
3. Decelerations
- Early Decelerations: Gradual and symmetrical decreases in FHR, typically associated with uterine contractions, often considered normal.
- Late Decelerations: Delayed and gradual decreases in FHR following uterine contractions, indicating potential fetal oxygenation issues.
4. Uterine Contractions
- Regular and Increasing Contractions: Consistent contractions with increasing intensity and frequency suggest progress toward active labor.
- Cervical Dilation and Effacement: As labor progresses, contractions contribute to cervical dilation and effacement.
Monitoring these patterns allows healthcare providers to gauge the well-being of both the fetus and the progress of labor. Understanding normal patterns and recognizing deviations helps ensure timely interventions if needed.
Identifying Abnormal Patterns
Identifying abnormal patterns in a fetal monitor is crucial for timely intervention and ensuring the well-being of both the mother and the baby. Here are indicators of abnormal patterns:
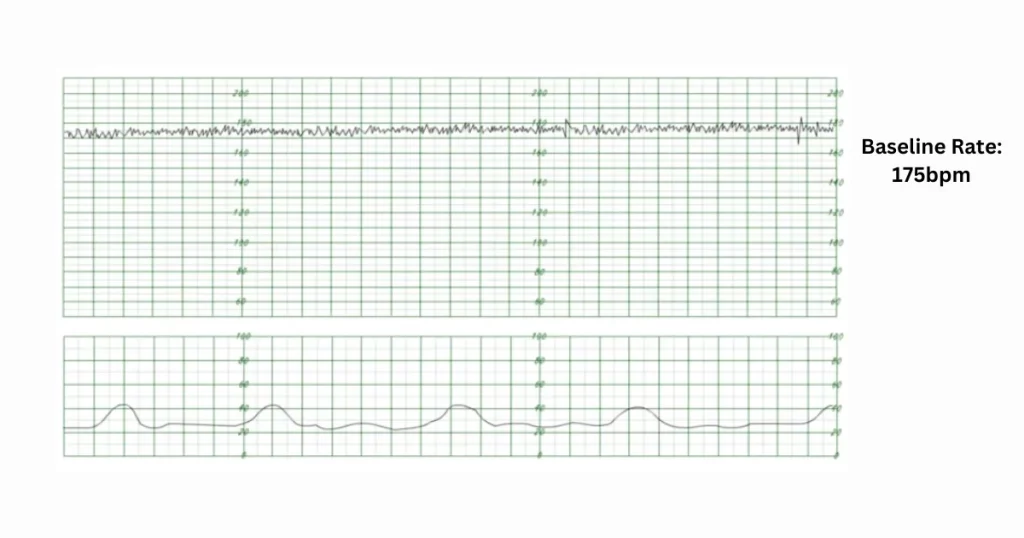
- Slow Fetal Heart Rate (Bradyarrhythmia): Persistent bradyarrhythmia, characterized by a consistently slow fetal heart rate below the normal range, may indicate fetal distress.
- Rapid Fetal Heart Rate (Tachyarrhythmia): Persistent tachyarrhythmia, with a consistently elevated fetal heart rate above the normal range, may suggest fetal distress.
- Reduced or Absent Fluctuations: A lack of variability in the fetal heart rate may indicate potential issues with fetal oxygenation and central nervous system function.
- Abrupt Decreases in FHR: Variable decelerations, characterized by abrupt and temporary drops in the fetal heart rate, may indicate cord compression or other fetal distress.
- Extended Reduction in FHR: Prolonged decelerations lasting more than three minutes may signify compromised fetal well-being and the need for further assessment.
- Meconium-Stained Amniotic Fluid: Presence of meconium in the amniotic fluid may indicate fetal distress.
- Late Decelerations: Gradual decreases in FHR occurring after the peak of uterine contractions may suggest inadequate oxygenation.
- Fluctuating or Unstable Fetal Heart Rate: An erratic baseline may indicate potential issues requiring attention.
Healthcare providers closely monitor these abnormal patterns, promptly addressing any concerns to optimize maternal and fetal outcomes during labor and delivery. Regular assessments and timely interventions contribute to a safer birthing experience.
Interpreting Variability in Fetal Heart Rate
Interpreting variability in fetal heart rate (FHR) is a critical aspect of fetal monitoring during pregnancy. FHR variability refers to the fluctuations in the fetal heart rate over time, and it provides valuable insights into the well-being of the fetus. Here are key points for understanding and interpreting FHR variability:
1. Normal Variability
- Fluctuations in Beats per Minute (bpm): A normal FHR exhibits variability, with fluctuations in beats per minute, reflecting the responsiveness of the fetal heart to the autonomic nervous system.
2. Absence of Variability
- Concern for Fetal Well-being: The absence or minimal variability in FHR may raise concerns about fetal well-being, as it may indicate potential issues with oxygenation and central nervous system function.
3. Categories of FHR Variability
- Short-Term Variability (STV): These are fluctuations that occur over a short duration, usually with a cycle length of 30 seconds to 2 minutes.
- Long-Term Variability (LTV): These are slower fluctuations that occur over longer periods, typically lasting more than 2 minutes.
4. Interpretation of Variability
- Moderate Variability: Moderate, irregular fluctuations within a normal range (6-25 bpm) are considered reassuring and indicative of a healthy fetal nervous system.
- Marked Variability: Excessive or marked variability may be associated with fetal distress or increased fetal activity.
5. Non-Reassuring Patterns
- Decreased Variability: Reduced or absent variability may be a sign of potential fetal compromise, and further assessment is warranted.
- Flat Tracing: A flat tracing with minimal or no fluctuations is concerning and requires immediate attention.
6. Factors Influencing Variability
- Gestational Age: FHR variability tends to increase with gestational age.
- Fetal Sleep State: Variability is often reduced during fetal sleep.
Interpreting FHR variability involves considering multiple factors and patterns. Healthcare providers carefully analyze these fluctuations to assess fetal well-being, guiding decisions for optimal maternal and fetal outcomes during pregnancy and labor. Regular monitoring and timely interventions contribute to a safer pregnancy and delivery experience.
Preparing for Different Stages of Labor
Preparing for different stages of labor in fetal monitoring involves adapting to the changing dynamics of the birthing process. Fetal monitoring is a crucial component of prenatal care, especially during labor, to ensure the well-being of both the mother and the baby. Here are key considerations for preparing and adjusting fetal monitoring strategies for different stages of labor:
1. Early Labor (Intermittent Monitoring): In the early stages, when contractions are mild and infrequent, intermittent monitoring may be employed. This involves periodic assessments of fetal heart rate (FHR) and uterine contractions to gauge overall well-being.
2. Active Labor (Continuous Monitoring): As labor progresses into the active phase with stronger and more frequent contractions, continuous electronic fetal monitoring (EFM) becomes more common. This provides a real-time, continuous assessment of FHR and uterine activity, offering a more detailed picture.
3. Transition Phase (Vigilant Monitoring): The transition phase, characterized by intense contractions and rapid cervical dilation, requires vigilant monitoring. Continuous EFM helps detect changes in FHR patterns and facilitates timely interventions if needed.
4. Second Stage (Pushing): During the pushing phase, intermittent monitoring may be combined with continuous monitoring to assess FHR between contractions. This ensures a balance between effective pushing and monitoring the baby’s well-being.
5. C-Section Preparation (Preoperative Monitoring): In cases where a cesarean section is planned or becomes necessary, preoperative fetal monitoring ensures the baby’s stability before the procedure. Continuous EFM is commonly used during C-sections.
6. Post-Delivery Assessment: After delivery, immediate assessment of the newborn’s condition is essential. Fetal monitoring may transition to neonatal monitoring, including Apgar scores and other assessments.
7. Adapting to Individual Needs: Throughout labor, healthcare providers adapt monitoring strategies based on individual factors, such as maternal health, fetal condition, and the progress of labor. Flexibility is key to providing personalized care.
Adapting fetal monitoring to different stages of labor requires a dynamic and individualized approach. Healthcare providers carefully assess the evolving needs of both the mother and the baby, ensuring a comprehensive and supportive birthing experience.
Final Words
Decoding contractions on the fetal monitor patterns is a skill that benefits both healthcare professionals and expectant parents. Regular monitoring, coupled with a clear understanding of the patterns, contributes to safe and informed decisions during labor, promoting the well-being of both the mother and the baby.